Table of Content
- Legal and Ethical Considerations
- Situations Where CPR Should Not Be Performed
- Additional Considerations
Cardiopulmonary resuscitation (CPR) is a critical life-saving technique that can dramatically improve survival rates during cardiac emergencies. According to the American Heart Association, effective bystander CPR can double or triple a victim’s chance of survival. CPR is often crucial in emergencies, but there are specific situations where it should not be performed.
While CPR is essential for restarting the heart and maintaining blood flow to vital organs, performing it inappropriately can be harmful or even fatal. For instance, a report from the National Institutes of Health (NIH) highlights that CPR is not recommended for individuals with do-not-resuscitate (DNR) orders or in cases where death is evident, such as severe trauma or prolonged illness.
This blog aims to educate readers on the scenarios where CPR should not be administered. By understanding when CPR is inappropriate, we can ensure it is used effectively and safely, providing the best possible outcomes for those in need
Legal and Ethical Considerations
Do Not Resuscitate (DNR) Orders
A Do Not Resuscitate (DNR) order is a legally binding document that indicates a person’s wish not to receive CPR if their heart stops beating or they stop breathing. These orders are usually part of a patient’s advanced directives and are critical in guiding healthcare professionals during emergencies.
Respecting Advanced Directives and Living Wills
Advanced directives and living wills are legal documents that outline a person’s preferences for medical treatment if they become incapacitated. They ensure that individuals receive care that aligns with their values and wishes. Respecting these directives is not only a matter of legal compliance but also an ethical obligation to honor the patient’s autonomy and decisions.
Legal Implications of Ignoring DNR Orders
Ignoring DNR orders can have serious legal repercussions. Healthcare providers who perform CPR on a patient with a valid DNR order may face legal action from the patient’s family or legal representatives. It can also lead to disciplinary measures by medical boards and loss of professional licenses. Ensuring that DNR orders and other advanced directives are followed is crucial for legal and ethical practice in CPR.
Situations Where CPR Should Not Be Performed
Presence of a DNR Order
A Do Not Resuscitate (DNR) order is a medical directive that clearly states a patient’s wish to forgo CPR if their heart stops or they stop breathing. These orders are typically established by patients who have terminal illnesses or conditions where resuscitation would not improve their quality of life.
A DNR order is a critical component of a patient’s healthcare plan, particularly for those with serious, chronic, or terminal conditions. It allows patients to make informed decisions about their end-of-life care, ensuring that their treatment preferences are respected.
How to Identify a DNR Order?
DNR orders are usually documented in the patient’s medical records and often come with a physical indicator, such as a bracelet, necklace, or a specific form that healthcare professionals can recognize quickly. In many places, this form is standardized for easy identification.
1. Respecting Patient Wishes
Respecting a DNR order is an ethical and legal responsibility for all healthcare providers. It is crucial to honor the patient’s wishes and avoid unnecessary and potentially distressing interventions. Healthcare professionals must be trained to recognize DNR orders promptly and act accordingly to respect the patient’s end-of-life preferences
2. Obvious Signs of Death
Certain conditions indicate that resuscitation efforts would be futile and inappropriate. Rigor mortis, or the stiffening of the body after death, is a clear sign that the person has been deceased for some time. Other signs include decapitation or decomposition, where the body shows evident signs of decay.
In these cases, initiating CPR would not be effective and could be distressing for both the responders and any onlookers. Recognizing these signs helps ensure that resources are used effectively and respectfully.
Attempting resuscitation in these situations is not only medically futile but can also be seen as disrespectful to the deceased and distressing to those present. Healthcare professionals are trained to recognize these signs and make appropriate decisions about the futility of CPR.
3. Unsafe Environment
Ensuring the safety of the rescuer is paramount before attempting any form of emergency intervention, including CPR. Responders should always assess the scene for potential hazards. If the environment poses significant risks, such as fire, toxic fumes, or unstable structures, it is critical to prioritize their own safety.
Examples of Unsafe Environments
Examples include
- Areas with active fires
- Exposure to toxic chemicals
- Locations that are structurally compromised.
In such scenarios, attempting to perform CPR without addressing these hazards first can put the rescuer’s life at risk.
Read More: What are the Common Myths and Misconceptions about CPR?
Prioritizing Getting Professional Help
In unsafe environments, it is crucial to call for professional emergency services immediately. Trained professionals with the appropriate equipment and protective gear are better suited to handle such situations. Responders should focus on getting help while ensuring their own safety.
4. Mass Casualty Incidents
In mass casualty events, where the number of injured individuals exceeds the available medical resources, triage protocols are essential. Triage involves prioritizing patients based on the severity of their conditions and their likelihood of survival with immediate medical intervention.
Focus on Victims with a Higher Chance of Survival
During triage, medical responders categorize victims into different groups. Priority is given to those with injuries that are severe but treatable, and who have the best chance of survival with prompt medical care. This often means that individuals with catastrophic injuries or those who are already deceased are not given immediate CPR, as the focus must be on maximizing the number of survivors.
Effective management of a mass casualty incident requires seamless coordination with emergency services. This coordination ensures that patients are quickly assessed, prioritized, and transported to appropriate medical facilities. Emergency services play a crucial role in implementing triage protocols and ensuring that resources are used efficiently to save as many lives as possible.
5. Traumatic Injuries Incompatible with Life
Certain traumatic injuries are so severe that survival is virtually impossible. Examples include massive head trauma, decapitation, or the complete severance of body parts. Recognizing these injuries is critical for responders to make informed decisions about when CPR is futile.
Understanding When Injuries Are Beyond the Help of CPR
In situations where injuries are clearly incompatible with life, performing CPR would not only be ineffective but could also divert attention and resources away from other victims who might benefit from immediate medical intervention. It’s essential for responders to understand when efforts are better spent on other patients.
Clear and effective communication with emergency responders is vital in these scenarios. Informing them about the nature and extent of the injuries helps ensure that appropriate decisions are made swiftly. This communication helps in the efficient allocation of resources and in providing the best possible care to those who can benefit from it.
6. Cardiac Arrest Due to Hypothermia
In cases of hypothermia-induced cardiac arrest, traditional resuscitation methods may not be effective. Cold temperatures can slow down bodily functions, including the heart rate, and increase the likelihood of survival. CPR should still be initiated, but medical responders must be prepared for unique challenges associated with hypothermia.
How Hypothermia Can Mimic Death?
Severe hypothermia can cause a person to appear lifeless, with a slow or undetectable pulse and shallow breathing. In such cases, it’s crucial not to mistake hypothermia-induced unconsciousness for death. Proper assessment and recognition of hypothermia symptoms are essential before determining the need for CPR.
In cases of hypothermia, immediate attention should be given to rewarming the individual. This may involve removing wet clothing, providing warm blankets, and applying external heat sources. CPR should only be initiated if there are no signs of circulation after rewarming efforts have been initiated.
7. Terminal Illnesses
When to Consider the Quality of Life and Patient Comfort?
In cases of terminal illness, where the prognosis is poor and the focus shifts from curative to palliative care, decisions about CPR become more complex. It’s essential to prioritize the patient’s comfort and quality of life, rather than aggressive life-saving measures that may offer little benefit.
Healthcare professionals, including physicians and palliative care specialists, play a crucial role in guiding end-of-life care decisions. Discussions about CPR should involve these professionals, who can provide insights into the patient’s prognosis, treatment options, and preferences regarding end-of-life care.
Balancing Hope and Realism in Terminal Cases
In terminal cases, it’s essential to strike a balance between maintaining hope and acknowledging the reality of the situation. CPR may not always align with the patient’s goals or wishes for their end-of-life care. Open and honest communication with patients, their families, and healthcare providers is key to making informed decisions in terminal cases.
Additional Considerations
No two medical emergencies are exactly alike, and it’s crucial to approach each situation with careful consideration of the circumstances. Factors such as the patient’s medical history, current condition, and the presence of advanced directives must all be taken into account when determining the appropriateness of CPR. Rapid assessment and critical thinking skills are essential in making informed decisions about CPR administration.
Consulting with Medical Professionals When in Doubt
When faced with uncertainty about whether CPR is appropriate, it’s always advisable to seek guidance from medical professionals. Physicians, nurses, and other healthcare providers can offer valuable insights and expertise based on their clinical judgment and experience. Consulting with medical professionals can help ensure that CPR decisions are aligned with the patient’s best interests and medical needs.
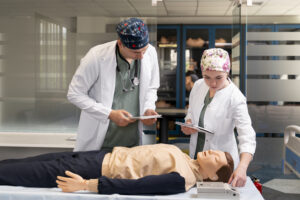
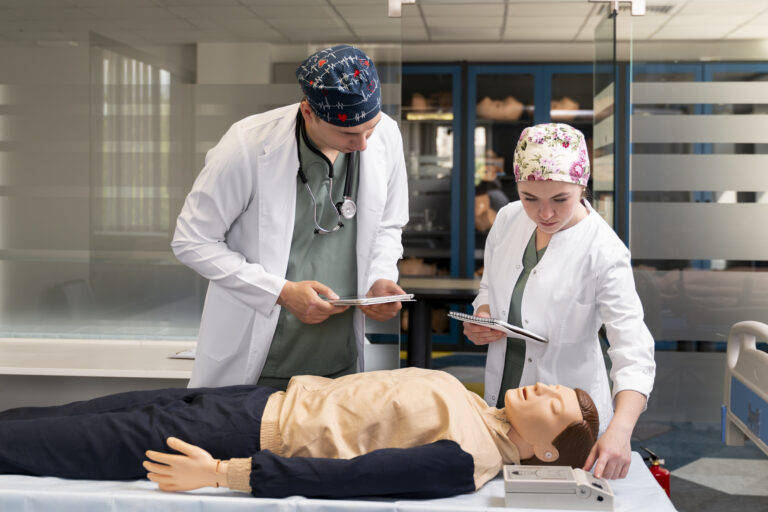
Maintaining up-to-date knowledge and skills in CPR is essential for all individuals involved in emergency response. Regular training and certification courses help ensure that responders are equipped to handle cardiac emergencies effectively and confidently. CPR guidelines and protocols may evolve over time, so staying informed through continuous education is key to providing the highest standard of care.
Read More: How to Perform Hands-Only CPR
Conclusion
In this guide, we’ve explored critical considerations for determining when not to perform CPR. Understanding situations such as the presence of a Do Not Resuscitate order, obvious signs of death, and unsafe environments is essential. By recognizing these scenarios, individuals can provide the most appropriate care to those in need.
Proper training and certification in CPR are crucial. Through ongoing education and certification courses, individuals can ensure they possess the necessary skills to respond effectively to emergencies while also understanding when CPR may not be appropriate.
We encourage everyone to seek further information and certification in CPR. Staying informed about CPR guidelines, consulting with medical professionals when uncertain, and maintaining certification are vital steps in being prepared to respond to emergencies and potentially save lives.
Frequently Asked Questions
You should avoid performing CPR if the person shows obvious signs of life, such as breathing or movement, or if there are clear signs of irreversible death, such as rigor mortis.
No, if you suspect a spinal injury, avoid performing CPR unless absolutely necessary. Incorrect handling can worsen the injury. Seek professional medical help immediately.
No, do not perform CPR if the environment poses a danger to you or the victim. Prioritize your safety and try to move to a safer location if possible.