Table of Content
- What is the Definition and Purpose of the Good Samaritan Law?
- Scope of Protection
- Legal Considerations for CPR Providers
- Tips for CPR Providers
- Good Samaritan Law by State:
Bag-mask ventilation is a fundamental technique used in emergency medical care to provide temporary respiratory support to patients who are unable to breathe adequately on their own. According to a study published in the “American Journal of Emergency Medicine,” approximately 50% of critically ill patients require some form of ventilatory support upon arrival at the emergency department. This underscores the significance of mastering bag-mask ventilation techniques for healthcare providers.
Bag-mask ventilation involves manually delivering breaths to a patient using a self-inflating bag connected to a face mask. This technique is employed when a patient’s spontaneous breathing is insufficient or absent. The bag is squeezed to deliver a tidal volume of air into the patient’s lungs, simulating the normal breathing process. This method ensures adequate oxygenation and ventilation while other interventions are initiated.
Understanding how breaths are delivered using a bag-mask device is paramount for healthcare professionals. By mastering this technique, they can confidently intervene during critical moments, potentially saving lives.
Components of a Bag-Mask Device
Bag-mask ventilation relies on several key components working together seamlessly to deliver breaths effectively. Understanding each component and its function is vital for proper utilization of the device:
1. Mask: The mask is a crucial part of the bag-mask device, creating a seal over the patient’s face to ensure that the delivered breaths go directly into the airway. It comes in various sizes to accommodate different patient populations, ensuring a snug fit and minimizing air leakage.
2. Bag: The self-inflating bag, typically made of silicone or other flexible materials, serves as the reservoir for the oxygen or air that is manually squeezed to deliver breaths to the patient. It must be sufficiently sized to deliver an appropriate tidal volume with each compression.
3. Valve: The valve system within the bag-mask device plays a vital role in controlling the direction of airflow. It ensures that when the bag is compressed, air flows only into the patient’s airway, preventing backflow of exhaled air or other contaminants. The valve also allows for the release of excess pressure, preventing barotrauma to the patient’s lungs.
Function of Each Component:
- The mask creates a seal, directing the delivered breaths into the patient’s airway.
- The bag serves as a reservoir for oxygen or air and is squeezed to deliver breaths.
- The valve system ensures unidirectional airflow and prevents contamination or barotrauma
Importance of Proper Assembly and Maintenance:
Proper assembly and regular maintenance of the bag-mask device are essential to ensure its functionality during emergency situations. Any leaks or malfunctions in the components can compromise ventilation efficacy, potentially leading to inadequate oxygenation and ventilation of the patient. Regular checks, cleaning, and replacement of worn-out components are necessary to maintain the device’s effectiveness and reliability. Healthcare providers must be trained in assembling and maintaining the bag-mask device to guarantee its readiness for use when needed most.
Preparing the Patient and Equipment
Effective bag-mask ventilation begins with proper preparation of both the patient and the equipment, ensuring optimal outcomes during emergency interventions:
1. Positioning the Patient:
Positioning the patient correctly is crucial for facilitating optimal ventilation. The patient should ideally be lying flat on their back on a firm surface. Tilting the head slightly backward and placing a small towel or pad under the shoulders can help align the airway, making it easier to ventilate.
2. Selecting the Appropriate Mask Size:
Choosing the right mask size is essential for achieving a proper seal and ensuring efficient delivery of breaths. Masks come in various sizes, ranging from pediatric to adult, and selecting the appropriate size based on the patient’s age and facial dimensions is critical. A mask that is too small may not create an adequate seal, leading to air leakage, while a mask that is too large may be uncomfortable for the patient and compromise ventilation effectiveness.
3. Ensuring a Proper Seal:
Achieving a proper seal between the mask and the patient’s face is paramount for effective ventilation. Before applying the mask, ensure that the patient’s face is clean and free from any obstructions or debris. Place the mask over the nose and mouth, making sure it covers both adequately. Then, using both hands, gently press down on the mask to form a seal, ensuring that no gaps exist between the mask and the skin. Verify the seal by observing chest rise and fall with each ventilation.
By following these steps to prepare both the patient and the equipment, healthcare providers can optimize the delivery of breaths during bag-mask ventilation, enhancing patient outcomes in emergency situations.
Bag-Mask Ventilation Technique
Mastering the bag-mask ventilation technique is essential for healthcare providers to effectively deliver breaths to patients in emergency situations. Here’s a step-by-step guide along with a demonstration of the “C-E grip” technique for optimal ventilation:
Positioning and Preparation:
Ensure the patient is correctly positioned on a firm surface with the head slightly tilted backward.
Select the appropriate mask size based on the patient’s age and facial dimensions.
Ensure a proper seal by aligning the mask over the nose and mouth and pressing down gently to create a seal.
C-E Grip Technique:
Hold the mask using the “C-E grip” technique, where the thumb and index finger form a “C” shape around the mask while the remaining fingers form an “E” shape around the mandible.
This technique helps in achieving a secure seal and allows for better control and stability during ventilation.
Delivering Breaths:
Squeeze the self-inflating bag with a firm, steady motion to deliver a breath.
Watch for chest rise and fall to ensure effective ventilation.
Aim for a tidal volume sufficient to produce visible chest rise but avoid overinflation to prevent barotrauma.
Timing and Frequency:
Deliver breaths at a rate of approximately 10 to 12 breaths per minute for adults and children.
For infants cpr, the rate may be slightly higher, around 20 to 30 breaths per minute.
Coordinate breath delivery with chest compressions during cardiopulmonary resuscitation (CPR) according to current guidelines.
Monitoring and Adjustments:
Continuously monitor the patient’s response to ventilation, including chest rise, oxygen saturation, and overall clinical status.
Make adjustments as needed, such as adjusting mask position or size, to ensure optimal ventilation and patient comfort.
By following these steps and mastering the C-E grip technique, healthcare providers can confidently and effectively deliver breaths using a bag-mask device, contributing to improved patient outcomes in emergency settings.
Monitoring and Adjustments
Monitoring the patient’s response during bag-mask ventilation is crucial for ensuring adequate oxygenation and ventilation. Here’s why it’s important, along with signs of effective ventilation and troubleshooting common issues:
Importance of Monitoring:
Continuous monitoring allows healthcare providers to assess the effectiveness of ventilation and make timely adjustments as needed.
Monitoring helps detect signs of inadequate ventilation, such as hypoxia or hypercapnia, and allows for prompt intervention to prevent complications.
Signs of Effective Ventilation:
Chest Rise: Visible chest rise with each breath indicates that air is entering the lungs and ventilating the patient effectively.
Oxygen Saturation (SpO2): Monitoring SpO2 levels provides real-time feedback on the patient’s oxygenation status. A stable or improving SpO2 suggests effective ventilation.
Patient Response: Observing the patient for signs of improvement in consciousness, color, and respiratory effort indicates successful ventilation.
Troubleshooting Common Issues:
Air Leaks: If air is escaping around the mask, check for proper mask placement and seal. Adjust the mask or try a different size if necessary. Ensure that the “C-E grip” technique is being used to maintain a secure seal.
Gastric Distention: Excessive air delivery can lead to gastric distention, causing discomfort and compromising ventilation. Reduce the volume and pressure of each breath delivered or consider alternative ventilation methods if gastric distention persists.
Obstruction or Blockage: Check for any obstructions in the airway that may impede ventilation, such as mucus or foreign objects. Clear the airway as needed and reassess ventilation effectiveness.
By actively monitoring the patient’s response and promptly addressing any issues that arise, healthcare providers can ensure optimal ventilation and improve patient outcomes during bag-mask ventilation in emergency situations.
Training and Certification
Proper training and certification in bag-mask ventilation are paramount for healthcare providers to deliver effective and lifesaving care. Here’s why it’s crucial, along with information on available courses and the importance of continual education:
Importance of Proper Training:
Competency and Confidence: Training ensures healthcare providers are proficient in bag-mask ventilation techniques, instilling confidence in their ability to manage airway emergencies effectively.
Patient Safety: Proper training reduces the risk of complications associated with inadequate ventilation, such as hypoxia or aspiration, safeguarding patient safety and well-being.
Availability of Courses and Certification Programs:
Basic Life Support (BLS) Courses: Many organizations offer BLS courses that include training in bag-mask ventilation as part of resuscitation protocols. These courses are widely available and cater to healthcare providers at various skill levels.
Advanced Training Programs: Advanced courses, such as Advanced Cardiovascular Life Support (ACLS) or Pediatric Advanced Life Support (PALS), provide in-depth training in airway management techniques, including bag-mask ventilation, for specific patient populations and clinical scenarios.
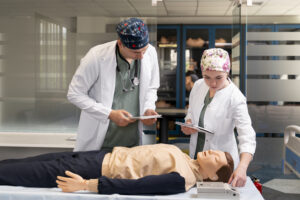
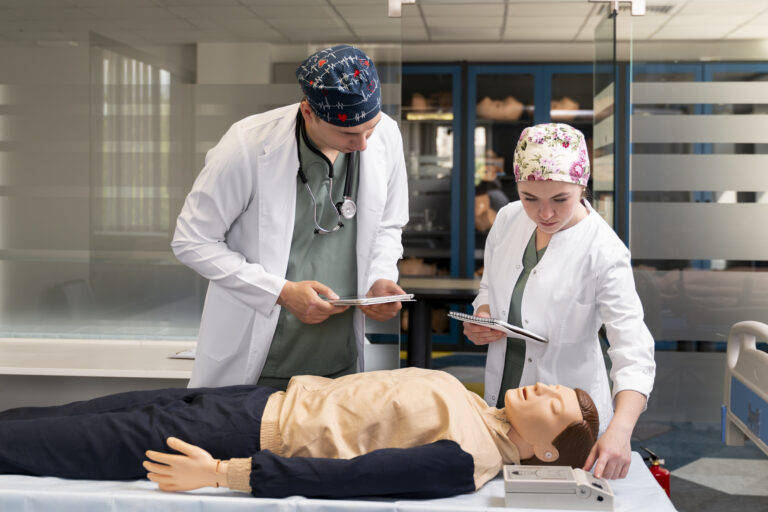
Simulation Training: Simulation-based training offers realistic scenarios for healthcare providers to practice bag-mask ventilation skills in a controlled environment, enhancing retention and proficiency.
Continual Education and Skill Maintenance:
Regular Refreshers: Healthcare providers should participate in regular refresher courses to reinforce bag-mask ventilation skills and stay updated on current guidelines and best practices.
Skill Drills: Conducting regular skill drills and simulations allows healthcare providers to practice and maintain proficiency in bag-mask ventilation techniques, ensuring readiness to respond to emergencies effectively.
Continuing Education: Stay informed about advancements in airway management and resuscitation through continuing education opportunities, conferences, and online resources to enhance knowledge and skills.
By investing in proper training, certification, and ongoing education, healthcare providers can ensure they are well-equipped to perform bag-mask ventilation competently and confidently, ultimately improving patient outcomes in emergency situations.
Conclusion
Effective bag-mask ventilation hinges on mastering proper technique and receiving adequate training. Key points include selecting the appropriate mask size, ensuring a proper seal, and delivering breaths using the C-E grip technique. Vigilant monitoring and prompt adjustments are crucial, especially for pediatric and infant patients, to prevent complications. Proper training and certification are essential, offering healthcare providers the competency and confidence needed to manage airway emergencies effectively. Continual education and skill maintenance through refresher courses and ongoing learning opportunities are encouraged to stay updated on best practices and advancements. By prioritizing proper technique, training, and ongoing education, healthcare providers can ensure optimal outcomes for patients requiring bag-mask ventilation in critical situations.
Frequently Asked Questions
A bag-mask device is a manual resuscitator used to provide breaths to patients in respiratory distress by squeezing the bag to push air through the mask into the patient's lungs.
A bag-mask device should be used during respiratory emergencies, such as cardiac arrest or severe respiratory failure, to ensure the patient receives adequate ventilation.
Key steps include positioning the mask securely over the patient's nose and mouth, sealing the mask with one hand, and squeezing the bag with the other hand to deliver breaths at a steady rate.